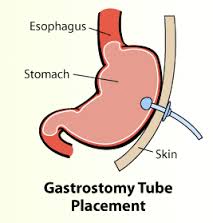
Gastrostomy Placement & Replacement
Gastrostomy tube (G-tube) placement (placing a tube into the stomach) to provide nutrition and medication for patients unable to feed themselves. G-tube placement routinely occurs with few complications when placed percutaneously using interventional radiology techniques.
Indications
A G-tube should be replaced as quickly as possible in the ED, unless the tube was recently placed. A feeding tube tract can narrow or close within hours of tube removal. A simple gastrostomy requires approximately 1-2 weeks to form a tract. More complicated procedures, such as the Witzel tunnel, may take 3 weeks to create a mature tract. If the tract appears fresh, immediately contact the provider who placed the tube before initiating ED replacement; operative or fluoroscopic replacement may be required.
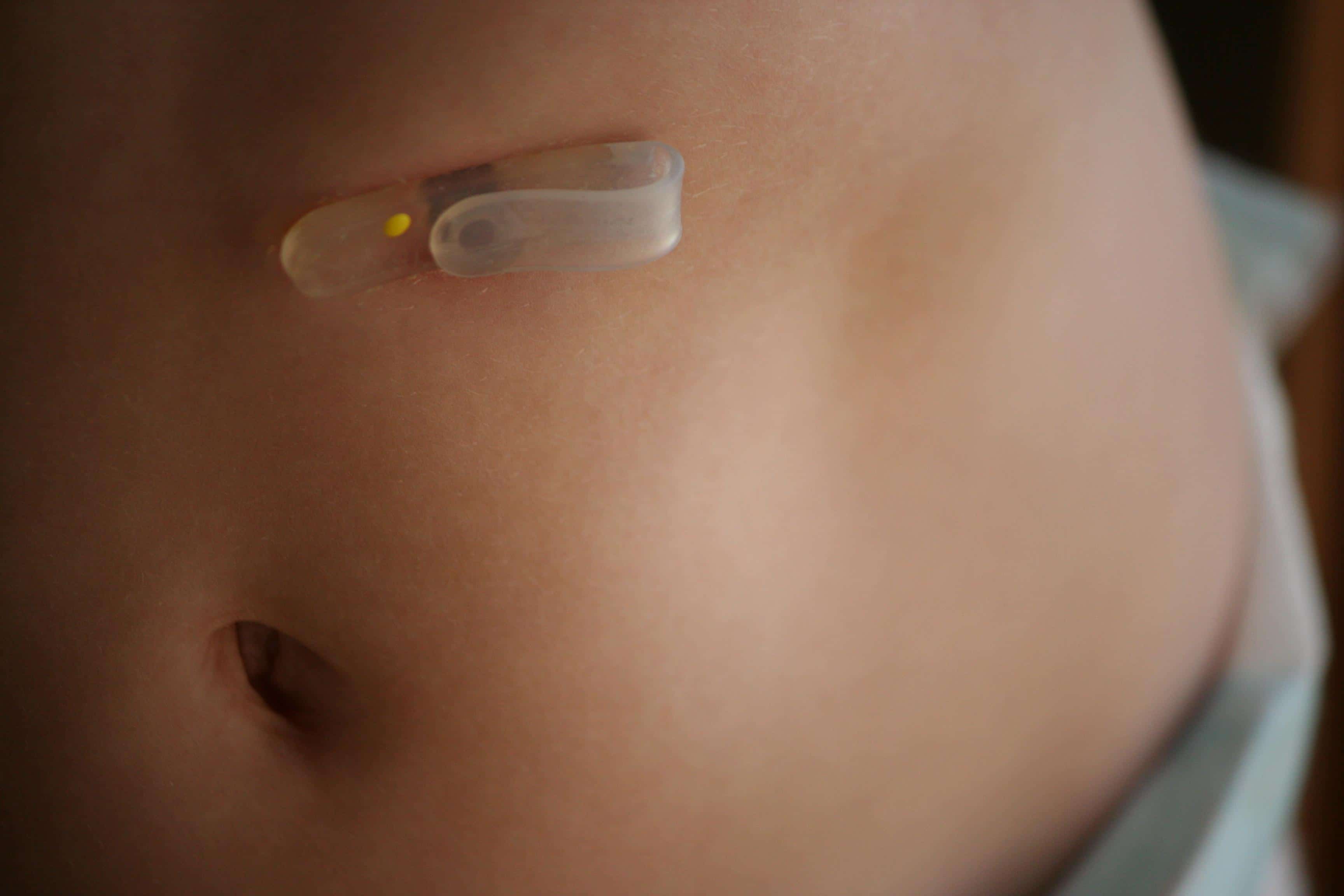
Gastrostomy Tube Removal
Often, the gastrostomy tube (G-tube) is only partially dislodged when the patient arrives in the emergency department (ED). In such cases, the tube must be removed prior to replacement. Not all G-tubes can be removed safely in the ED. Standard de Pezzer and mushroom catheters modified with rings or bolsters upon insertion may require endoscopy for removal. However, most G-tubes can be taken out with simple traction. When in doubt, contact the provider who inserted the tube to determine if removal can be completed safely in the ED. Of note, the visible portion of the G-tube outside the skin may or may not indicate what type of internal stabilization exists. G-tube removal begins with deflating the balloon, if one exists. Then, while providing traction on the tube, press a flat, gloved hand against the abdominal wall for countertraction. The tube should slide out with minimal resistance. If significant resistant is felt, the procedure should be aborted, as an internal ring or bolster that requires endoscopic removal may exist.
Gastrostomy Tube Replacement
Once the tube has been removed, replacement should occur as soon as possible to prevent tract narrowing and closure. If a similar G-tube will not pass through the tract or cannot be found, place a smaller tube or a Foley catheter to keep the tract open. A more permanent tube can be placed at a later time. Before using the G-tube is used for feedings, placement must be confirmed. Classically, confirmation is made by injecting 20-30 mL of water-soluble contrast solution (diatrizoate meglumine diatrizoate sodium) into the tube and taking a supine abdominal radiograph within 1-2 minutes. This is best performed in the radiography suite. Barium should never be used, because its injection into the peritoneal cavity can be devastating. The tube should slide out with minimal resistance. If significant resistance is felt, the procedure should be aborted, as an internal ring or bolster that requires endoscopic removal may exist.
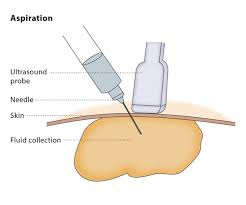
Percutaneous Drainage
Image-guided percutaneous drainage and aspiration procedures provide therapeutic treatment for many types of fluid collections, including abscess, hematoma, bulla, seroma, and cysts. Drainage treatment is defined as the placement of a catheter to provide complete or continuous drainage of the fluid collection. Aspiration treatment is defined as evacuation of a fluid collection or cyst, using either a needle or catheter, with immediate removal of the catheter or needle after the treatment.
Gastrostomy Tube Replacement
 You will be brought into the CT room and asked to lie on an X-ray table. A CT scan of your body will be taken to determine the best area of approach to the fluid collection of interest. The Radiologist will then clean off the skin, over the determined area of interest, with a special soap. You will be given numbing medication in the skin through a small needle. The Radiologist will then insert a small needle through the numbed area of skin and into the fluid collection. You may feel some pressure when this happens. Once the needle is in the right place, the fluid will then be removed. The needle will then be removed and your skin will be cleaned off again, and a Band-Aid will be applied over the spot.
You will be brought into the CT room and asked to lie on an X-ray table. A CT scan of your body will be taken to determine the best area of approach to the fluid collection of interest. The Radiologist will then clean off the skin, over the determined area of interest, with a special soap. You will be given numbing medication in the skin through a small needle. The Radiologist will then insert a small needle through the numbed area of skin and into the fluid collection. You may feel some pressure when this happens. Once the needle is in the right place, the fluid will then be removed. The needle will then be removed and your skin will be cleaned off again, and a Band-Aid will be applied over the spot.
Will It Hurt?
There may be some discomfort associated with this procedure. Many cases can be performed with a local anesthesia (similar to Novacaine used by dentists). More involved cases generally will require the administration of painkillers and/or anti-anxiety medications. The most involved procedures generally will involve insertion of a small intravenous line and monitoring by our Radiology nursing staff in order to administer medications intravenously. Every effort is made to minimize any discomfort during the procedure.
How Long Will It Take?
Interventional procedures in general last anywhere from 30-90 minutes, depending on the size of the area of interest and the amount of fluid being removed. This particular procedure will necessitate a post-procedure observation period of 1-4 hours to ensure no complications resulting from the procedure.
Thoracentesis & Paracentesis
 Paracentesis refers to a procedure to remove excess fluid via a needle syringe from a body cavity, most often the abdomen. Removal of fluid from the chest cavity is called thoracentesis. The causes of fluid buildup in the body are many, including liver disease, congestive heart failure, pneumonia, infections, and certain cancers. Draining the fluid relieves pressure on the patient’s internal organs which may cause more serious complications and provides a sample for diagnostic tests.
Paracentesis refers to a procedure to remove excess fluid via a needle syringe from a body cavity, most often the abdomen. Removal of fluid from the chest cavity is called thoracentesis. The causes of fluid buildup in the body are many, including liver disease, congestive heart failure, pneumonia, infections, and certain cancers. Draining the fluid relieves pressure on the patient’s internal organs which may cause more serious complications and provides a sample for diagnostic tests.
Treatments
Performed on an outpatient basis under local anesthesia, doctors insert a hollow needle with a plastic sheath into the abdomen, chest or affected area. This is done with the guidance of ultrasound imaging that helps doctors place the needle at the optimal location and depth and avoid other organs in doing so. Once in place, the doctor withdraws the needle, leaving the plastic sheath as an outlet for fluid drainage. Though very safe and generally painless, these procedures carry a very small risk of infection or bleeding. Afterwards, patients can return to normal activities.
Request an Appointment
For gastrostomy tube placement or replacement, make an appointment with our specialists for an evaluation. The experienced physicians at Precision Vascular and Interventional Radiology will create an individualized plan to help you get the best results.