What Is Hypertension?
The American College of Cardiology and the American Heart Association defines hypertension, or high blood pressure (BP), as:1
- elevated BP, with a top reading (called systolic pressure) between 120 and 129 mm Hg and the bottom number (called diastolic pressure) less than 80 mm Hg, and
- stage 1 hypertension, with the upper reading of 130 to 139 mm Hg or a lower reading of 80 to 89 mm Hg (i.e., ≥ 130/80 mm Hg)
The upper reading (systolic pressure) represents the phase when the heart squeezes to pump blood out into your arteries. The bottom number (diastolic pressure) occurs when the heart relaxes in between heartbeats.

What Is the Link between Hypertension and PAD?
Hypertension is one of the major yet modifiable risk factors for vascular disorders, including Peripheral Arterial Disease (PAD). There is a strong link between the two diseases. About 50% to 92% of patients who present with PAD are also found to have high blood pressures.2
Moreover, people with PAD whose blood pressures are persistently on the higher side, are not only at risk of complications of PAD like amputation and disability but also at risk of damage to major organs like heart and brain. In particular, a higher systolic BP (the numerator) reading makes you prone to heart disease and stroke.3

Does Hypertension Damage Your Arteries?
High Blood Pressure Places Tension on Arterial Walls
Knowing what exactly blood pressure is may help you perceive the mechanism of damage to your arteries when the pressure inside them grows. By definition, blood pressure is the force that the blood puts on the walls of your arteries. The blood flowing through your arteries should exert a normal amount of force on their walls so as to allow a continuous, uninterrupted flow of blood. However, if the BP remains high consistently, it will put extra strain on the arteries throughout your body, including the legs, causing them to narrow. This leads to characteristic PAD symptoms. In fact, the risk of developing the classical claudication (walking-calf pain) of PAD rises to 2.5- to 4-fold in both men and women with hypertension.2

High Blood Pressure Clogs the Arteries
Just like diabetes and high cholesterol levels, long-standing high blood pressure also leads to a buildup of plaque (fatty deposits) in the arteries of your legs. These plaque-clogged arteries harden and narrow, restricting the flow of blood through them. The medical term for this plaque buildup process is “atherosclerosis.”
Hypertension Has a Link to High Blood Cholesterol
Despite the arterial clogging due to hypertension, it is predominantly the buildup of fat in your blood that actually sets off the formation of plaque in your arteries. Moreover, dyslipidemia (the abnormal amounts of fat in your blood) often occurs along with hypertension. High blood cholesterol works in tandem with high blood pressure to damage your blood vessels and your heart even faster.
Consistently high bad cholesterol levels double your odds of developing high blood pressure and eventually your chances of heart and blood vessel diseases, including PAD. Even slightly raised cholesterol levels can impact the pressure required to shove blood through the blood vessels by impairing their squeezing and relaxing mechanisms.4
In view of this, it wouldn’t be surprising to say that abnormal amounts of bad cholesterol (LDL) and high blood pressure serve as the “partners in crime” to destroy your arteries.
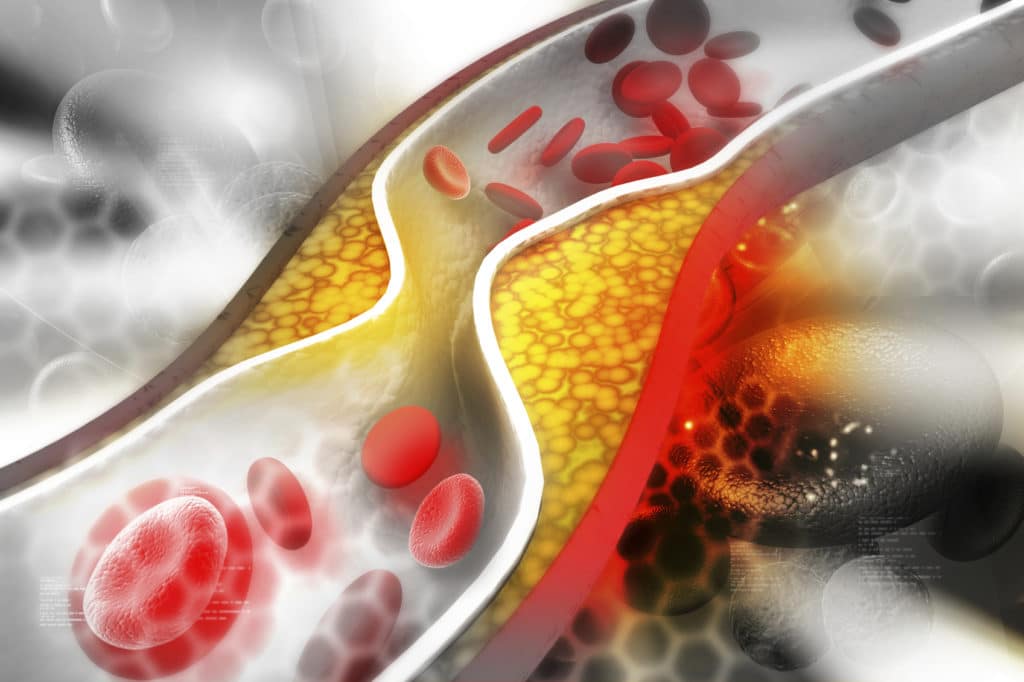
The steps of arterial damage in response to high blood pressure are thus much like the damage caused by high low-density lipoproteins (LDL) levels.
LDL Becomes Oxidized
When your blood contains abnormal amounts of LDL, the bad cholesterol can also build up in the walls of your arteries. This LDL is very susceptible to interact with destructive oxygen species called free radicals, after which, it turns into “oxidized” LDL—meaning an “unstable” LDL that has oxygen atoms attached to it.
Certain Blood Cells Devour LDL
The oxidized LDL is avidly taken up and gobbled by unique blood cells, which themselves transition into cells with a foamy appearance called foam cells. The foam cells which are the precursors to atherosclerosis amass to generate the so-called ‘fatty streak’ in your blood vessels.
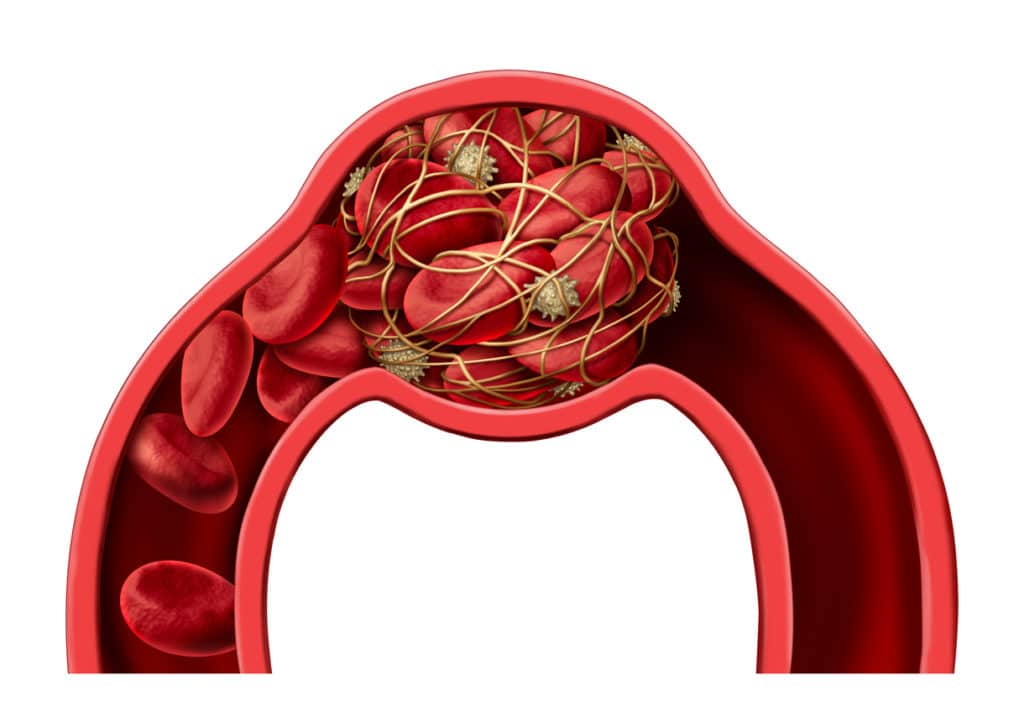
Platelets Get Activated and the Plaque Grows
Platelets are the blood cells that function to cease bleeding by forming a blood clot. When the fatty streak becomes of sufficient size, platelets stick to the underlying matrix. The activated platelets release a number of growth factors. These growth molecules cause the cells of blood vessels to expand and migrate towards the inner coat of your artery where the plaque resides. When that happens, the plaque gets bigger and becomes covered by a cap.
The Plaque Ruptures and Blood Clot Forms
The cap lacks strength and can easily rupture. Rupture of the cap exposes the underlying matrix to the blood, forming a blood clot that may occlude the vessel or become, once more, wrapped in a fiber-like coat, furthering the spread of the plaque. Blockage of a blood vessel supplying your legs and feet leads to the hallmark symptoms of PAD.
Does Treating High Blood Pressure Help PAD?
So, you see how high BP plays a critical role in damaging your arteries. Lowering BP in PAD shows promise in minimizing cardiovascular (heart and blood vessel) complications. Clinical trials carried out on people with PAD show a reduced frequency of cardiac and vascular events in those receiving blood pressure-lowering pills. Therefore, it is advised that PAD patients whose blood pressure is >140/90 be treated with BP medications to bring their numbers down.5
In some previously published clinical trials, PAD patients also reported an improvement in walking distance without pain after being placed on medications for high blood pressure (anti-hypertensives). The blood flow to the calf also appeared to improve in these individuals, further supporting the benefits of blood pressure medicines in people with PAD.5

Moreover, we know that diabetes also contributes to PAD, speaking of which, there is evidence that if the blood pressures are well controlled in these patients—then, this may help stem the tide of PAD.2 The goal is to keep the BP to less than 140/90 mm Hg (in people without diabetes) or below 130 mm Hg systolic over 80 mm Hg diastolic (if you also have diabetes or chronic kidney disease) to cut down your risk of heart attack, stroke, or cardiovascular death.6
Key Takeaway
Hence, the key to keeping your arteries unclogged is to maintain your blood pressure and cholesterol levels within a normal range. Keeping track of blood pressure at home is, therefore, essential. If you already have PAD, be sure to implement healthy lifestyle changes and check with your doctor regarding the BP medicines to prevent any further damage to your arteries.
Peripheral Artery Disease Screening
If you think you, a family member or friend has the symptoms of PAD, it is important to confirm the diagnosis and seek treatment. The experts at Precision Vascular and Interventional would be happy to discuss PAD with you in person. Book an appointment today by calling 214-382-3200 or complete the form below.
Precision VIR serves the DFW area including Dallas, Fort Worth, Carrollton, Richardson, Garland, Mesquite, Highland Park, University Park, Park Cities, Plano, Frisco, McKinney, Arlington, Irving, Grand Prairie, Denton, Lewisville and all of North Texas.
This information is not a substitute for professional medical advice. Prior to starting any new treatment or questions regarding a medical condition, always seek the advice of your doctor or other qualified health provider.
References
- American College of Cardiology. New ACC/AHA High Blood Pressure Guidelines Lower Definition of Hypertension. Retrieved June 18, 2019 from https://www.acc.org/latest-in-cardiology/articles/2017/11/08/11/47/mon-5pm-bp-guideline-aha-2017
- Olin JW, Sealove BA. Peripheral artery disease: current insight into the disease and its diagnosis and management. Mayo Clin Proc. 2010;85(7):678–692. doi:10.4065/mcp.2010.0133.
- Alique M, Luna C, Carracedo J, Ramírez R. LDL biochemical modifications: a link between atherosclerosis and aging. Food Nutr Res. 2015;59:29240. Published 2015 Dec 3. doi:10.3402/fnr.v59.29240.
- Ferrara LA, Guida L, Iannuzzi R, Celentano A, Lionello F. Serum cholesterol affects blood pressure regulation. J Hum Hypertens. 2002;16(5):337-43.
- Thomas Manapurathe D, Krishna SM, Dewdney B, Moxon JV, Biros E, Golledge J. Effect of blood pressure lowering medications on leg ischemia in peripheral artery disease patients: A meta-analysis of randomised controlled trials. PLoS One. 2017;12(6):e0178713. Published 2017 Jun 2. doi:10.1371/journal.pone.0178713.
- Rooke TW, Hirsch AT, Misra S, et al. Management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA Guideline Recommendations): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(14):1555–1570. doi:10.1016/j.jacc.2013.01.004.

