What Does a PAD Diagnosis Mean, and What Are My Options?
What Is PAD?
PAD, or peripheral artery disease, is a disease of the peripheral arteries—arteries that supply blood to the outer areas of your body, in particular, the legs. The key trigger is a buildup of plaque (fatty deposits) in the arteries of your legs, which hardens and narrows them and restricts the blood flow. Medically referred to as “atherosclerosis,” this is the same process that triggers heart disease. Hence, it’s not difficult to understand how the PAD and heart disease are related.
The reduced blood supply to your legs gives rise to the telltale features of PAD, especially the walking-calf pain called intermittent claudication.

The plaque can build up in peripheral arteries as a result of:
- Smoking
- Diabetes
- High blood cholesterol levels
- High blood pressure
- Obesity
- Having heart and blood vessel (cardiovascular) disease, or
- Having a relative with heart disease

The downside with many people having PAD is that they do not show any signs and symptoms, and the condition can go undiagnosed and untreated until complications ensue.
What Are The Stages Of PAD?
Initial Stages
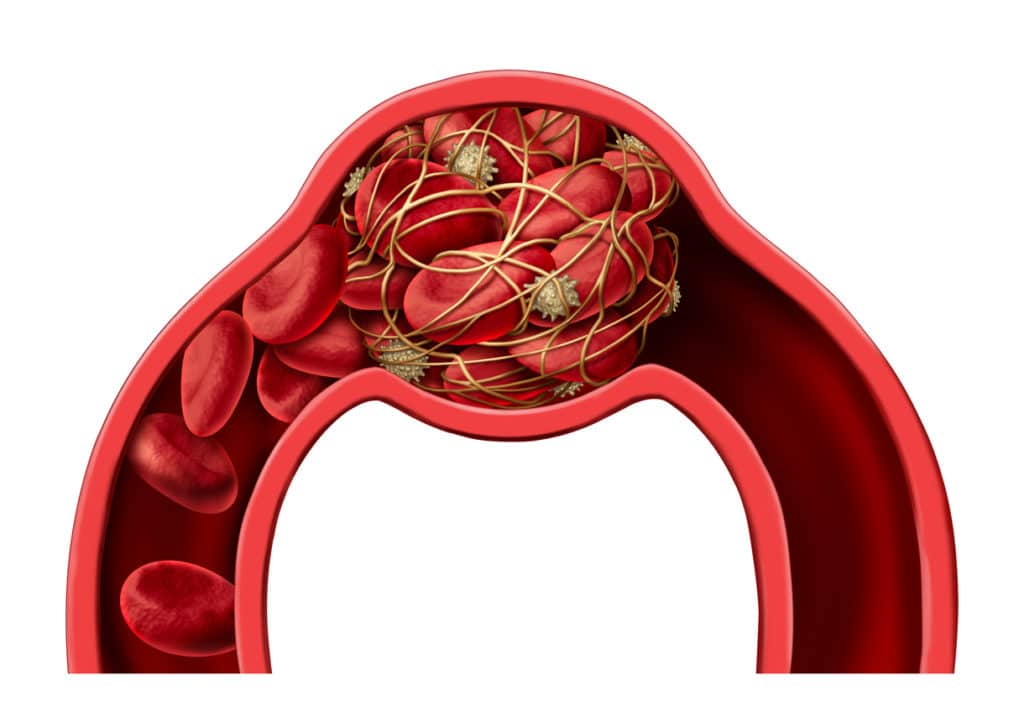
PAD can progress from no symptoms at all to a critical state of “no blood flow,” warranting an amputation. Initially, the sluggish blood flow will not cause any symptoms. But as the plaque starts to block the artery more and more, the claudication keeps getting worse. As the disease takes its course, the plaque can suddenly burst, forming a blood clot and completely blocking the blood flow to your leg.
Advanced Stages
Severe blockage of your arteries markedly reduces blood flow to your extremities, leading to severe pain at rest called “rest pain.” This marks the onset of a condition what we call “Critical Limb Ischemia (CLI),” causing pain that is severe enough to wake you up at night. Ischemia is an inadequate blood supply to a limb or organ. CLI is the advanced stage of PAD that calls for urgent intervention to restore blood supply and oxygen to the deprived leg. At this point, the pressure of the artery at your ankle called arterial pressure, or AP, is markedly dropped to the point where no pulsations can be detected at all. If you’ve been diagnosed with PAD, you must have undergone a test called ankle-brachial index (aka ABI). This test compares the arterial pressure at your ankle to the blood pressure in your arm. A lower ABI indicates more severe disease.
If left untreated, the lack of oxygen-rich blood causes the tissue of the affected limb to die and develop gangrene. This is obvious by the overlying skin turning black and the appearance of sores or blisters that bleed or emit foul-smelling pus. The gangrene can spread rapidly and thus needs to be removed as soon as possible to salvage the limb. More severe cases of gangrene warrant amputation (surgically removing the limb).
How Do Vascular Specialists Classify The Stages of PAD?
Doctors look at the stages of PAD in two ways.
A. Fontaine classification1
Dr. Fontaine classified PAD into four stages solely relying on clinical symptoms:
| Grade | Symptoms |
| Stage I | No symptoms, an artery is not completely blocked |
| Stage II | Mild claudication pain in limb |
| Stage IIA | Claudication at a distance > 200 meters |
| Stage IIB | Claudication at a distance < 200 meters |
| Stage III | Pain at rest |
| Stage IV | Necrosis (death) and/or gangrene of the limb |
B. Rutherford classification
The other way to determine the progression of your disease is by looking at the intensity of symptoms along with the results of exercise treadmill testing and ankle-brachial index (ABI). Dr. Rutherford took into account the symptoms of PAD together with the results of tests to classify the stage of peripheral vascular disease. This classification system consists of four grades and seven categories.1
| GRADE | CATEGORY | SYMPTOMS | RESULTS ON TESTING |
| 0 | 0 | No symptoms | Normal treadmill testing |
| 1 | Mild claudication | Completes treadmill exercise; arterial pressure (AP) after exercise > 50 mm Hg but at least 20 mm Hg lower than resting value | |
| I | 2 | Moderate claudication | Between categories 1 and 3 |
| 3 | Severe claudication | Cannot complete standard treadmill exercise, and AP after exercise < 50 mm Hg | |
| II | 4 | Ischemic rest pain | Resting AP < 40 mm Hg, pulsations barely detectable in the ankle |
| III | 5 | Minor tissue loss—nonhealing ulcer, gangrene with extensive foot ischemia | Resting AP < 60 mm Hg, flat or no pulsations in the ankle |
| IV | 6 | Major tissue loss—functional foot no longer salvageable | Same as category 5 |
What Are The Treatment Goals For PAD?
The treatment goals for PAD include:
- Addressing symptoms, such as calf pain, allowing you to resume physical activities
- Impeding the progression of PAD to reduce your risk of serious complications such as blood clots, amputation, heart attack, and stroke
What Are The Medical Alternatives To Help My Symptoms?
Medications to relieve your symptoms: Your doctor can prescribe medicines to control your claudication symptoms. These medicines improve the blood flow and oxygen supply to the affected limb by widening the blood vessels and keeping the blood thin. They show promise in improving the maximal walking distance in PAD.
Medicines to keep your blood thin and prevent blood clots in arteries: You will be put on a daily dose of blood-thinners like aspirin or clopidogrel (Plavix).
Medicines to control risk factors: If you have high blood pressure, blood sugar, or cholesterol levels, medicines to keep all these triggers under control will also be prescribed.
Lifestyle changes: like smoking cessation, a healthy diet, and enrolling in a supervised walking program will further help improve your walking distance, reduce body weight, and slow the rate of functional decline.

What If My Symptoms Don’t Respond To These Medical Therapies?
In cases where medical and exercise therapies fail or if you have lifestyle-limiting claudication symptoms, surgery is the next line of therapy.
Typically the surgical options for PAD include:
- Minimally invasive endovascular procedures like stenting, balloon angioplasty, or atherectomy
- Open bypass surgery
Today, vascular specialists prefer endovascular procedures over open surgery for treating PAD as they are minimally invasive, have fewer side effects, and are promising.
What Is The Role Of Angiography In PAD?
Before any surgical intervention for PAD, X-ray imaging with a contrast medium (dye) called angiography is done to visualize blood flow in the arteries of your legs. Angiography helps the surgeon identify the site and severity of blockage as well as the condition of blood vessels close to the blockage prior to surgically treating the narrowed arteries.
There are three different types of angiographies:
- Catheter angiography: The surgeon makes a cut in the skin of your groin and passes a balloon-tipped tube called catheter filled with contrast fluid (dye) over a thin guide wire through an artery in the groin.
- CT angiography: A CT scanner is used to provide images of arteries and blood vessels.
- Magnetic resonance angiography (MRA): is a type of magnetic resonance imaging (MRI). It is a non-invasive alternative to a traditional (catheter) angiogram. The MRA uses a magnetic field and radiofrequency waves to produce detailed images of blood vessels. You will be given a dye through a vein to improve the image quality and pinpoint the diseased areas more accurately.
What Are Minimally-Invasive Endovascular Treatments For PAD?
The two main types of endovascular treatments for PAD are:
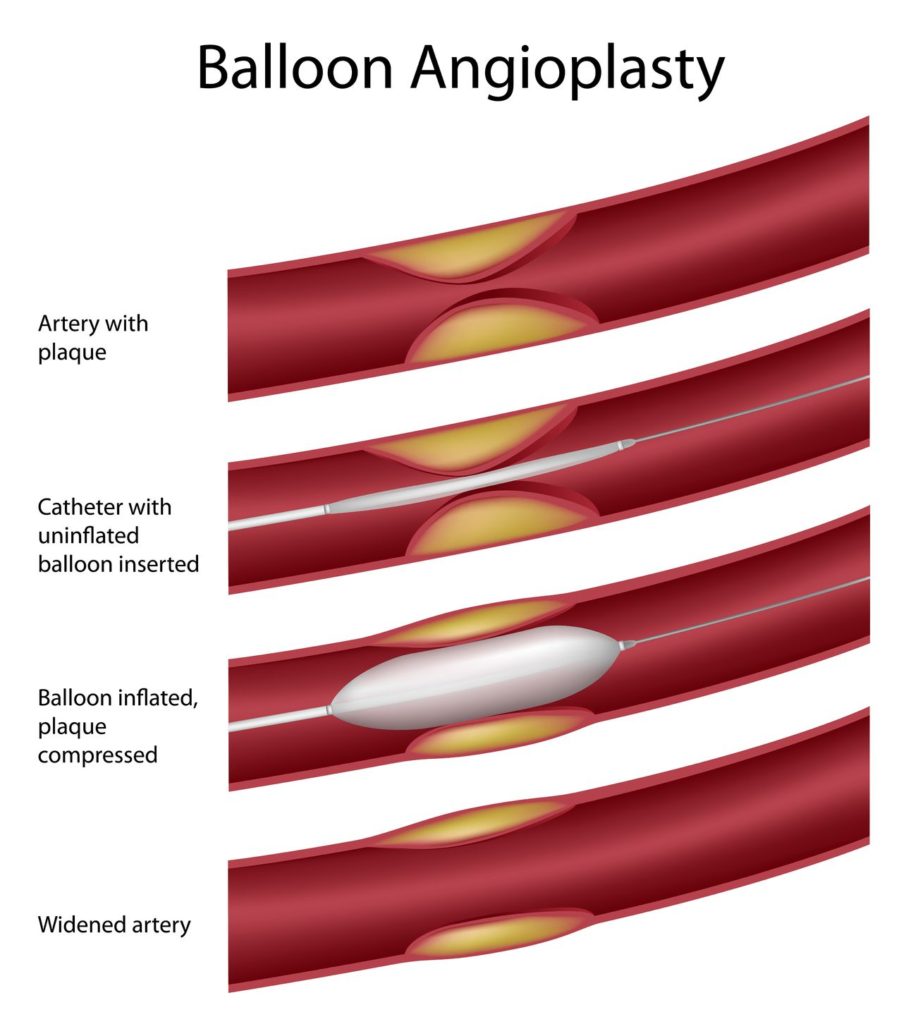
1. Balloon Angioplasty with Stenting:
As soon as the blockage site is identified via angiography, the balloon at the catheter tip is inflated that pushes the plaque against the wall of the artery. This widens the internal opening of the narrowed artery (or lumen) and improves blood flow. The balloon is then deflated and taken out.
In special circumstances, vascular specialists also place a drug-eluting balloon coated with a medicine to improve the patency of the recently expanded blood vessel. The goal of using this balloon is to minimize the chances of post-treatment narrowing of arterial diameter again. A stent (metal scaffold) may also be inserted to keep the artery open.
2. Atherectomy:
This is the surgical removal of atherosclerosis (plaque) from the affected peripheral arteries.
To carry out the procedure, a medicine to numb the area is given along with a mild sedative. Your surgeon will thread a catheter (equipped with a blade or laser at its tip) through the artery in the groin to the area of blockage. The surgeon then debulks and removes the plaque using various methods such as cutting, scraping or lasering. This enlarges the arterial diameter. The catheter may have to be moved back and forth several times to effectively remove a significant amount of plaque.
Your surgeon may perform atherectomy:
- alone, or
- together with balloon angioplasty to help place the stent or to improve patency without using a stent, or
- before carrying out balloon angioplasty to optimize the results and thus completely eliminate the plaque
What Is The Success Rate Of Angioplasty?
The technical success rate of angioplasty and/or stenting for upper leg peripheral artery disease exceeds 90%.2 Angioplasty improves mild to moderate claudication and walking distance at 6-months. However, benefits appear to be limited in the long-term.
What Is Bypass Surgery And Why Do I Need It?

A surgical bypass redirects blood flow from the blocked artery by creating an alternative passage for blood flow using a graft. It is a major surgical procedure done in an operation theater. To bypass the blockage, your surgeon will first make a cut right below the area of blockage in the damaged artery. A graft, which could be either a part of one of your leg veins or a synthetic blood vessel, is then connected above and below the blockage. By creating a separate channel for the blood to bypass the blockage, the new vessel (graft) restores the blood flow to the affected leg.
You may need this procedure if:
- Your doctor determines that the damage to your arteries is extensive and is unlikely to respond to less invasive procedures.
- Your prior angioplasty attempt failed to restore the blood supply.
- For severe claudication that fails to respond to a trial of medications and less invasive procedures.
Peripheral Artery Disease Screening
If you think you, a family member or friend has the symptoms of PAD, it is important to confirm the diagnosis and seek treatment. The experts at Precision Vascular and Interventional would be happy to discuss PAD with you in person. Book an appointment today by calling 214-382-3200 or complete the form below.
Precision VIR serves the DFW area including Dallas, Fort Worth, Carrollton, Richardson, Garland, Mesquite, Highland Park, University Park, Park Cities, Plano, Frisco, McKinney, Arlington, Irving, Grand Prairie, Denton, Lewisville and all of North Texas.
This information is not a substitute for professional medical advice. Prior to starting any new treatment or questions regarding a medical condition, always seek the advice of your doctor or other qualified health provider.
References
- Hardman RL, Jazaeri O, Yi J, Smith M, Gupta R. Overview of classification systems in peripheral artery disease. Semin Intervent Radiol. 2014;31(4):378–388. doi:10.1055/s-0034-1393976.
- O’Donnell ME, Reid JA, Lau LL, Hannon RJ, Lee B. Optimal management of peripheral arterial disease for the non-specialist. Ulster Med J. 2011;80(1):33–41.

